Early detection and proactive management are essential in improving cancer outcomes. While oncologists focus on tumor-specific therapies such as chemotherapy, radiation, or surgery, primary care providers play a complementary role in monitoring overall health, detecting warning signs, and supporting the patient’s broader wellness.
Cancer treatment can be overwhelming, both physically and emotionally. Patients often face multiple medications, frequent appointments, and complex treatment decisions. By integrating primary care into the oncology care team, clinicians can anticipate complications, address coexisting conditions, and ensure that patients maintain their overall health throughout treatment.
A holistic approach recognizes that cancer does not occur in isolation. Fatigue, nutritional challenges, chronic conditions like diabetes or hypertension, and mental health needs can all affect treatment effectiveness and recovery. Primary care providers act as a continuous thread, linking specialty care with preventive strategies, emotional support, and long-term wellness planning.
The Role of Primary Care in Early Detection
Primary care physicians are often the first point of contact when patients notice unusual symptoms. Regular check-ups, comprehensive physical exams, and routine screenings enable providers to identify early warning signs of cancer, such as persistent fatigue, unexplained weight loss, or abnormal lab results.
Grand Forks Clinic emphasizes preventive care and chronic disease management, helping patients maintain health baselines that make deviations more noticeable. For example, a long-term patient under routine monitoring may present subtle changes that could indicate a developing malignancy, allowing for timely referral to an oncologist.
Beyond detection, primary care providers coordinate diagnostic testing, imaging, and specialist consultations to ensure comprehensive care. This integrated approach ensures that patients move smoothly through the healthcare system without unnecessary delays, increasing the likelihood of early-stage treatment and better outcomes.
Chronic Conditions and Cancer Risk
Patients with chronic conditions such as diabetes, cardiovascular disease, or autoimmune disorders may face higher risks during cancer treatment. Poorly managed health can complicate chemotherapy, increase susceptibility to infections, and affect recovery times.
Primary care providers help manage these conditions proactively. Through medication optimization, lifestyle counseling, and regular monitoring, clinicians create a foundation for patients to tolerate aggressive cancer therapies more safely.
Integrating chronic disease management with oncology care also reduces hospitalization rates and treatment interruptions, improving overall quality of life. Preventing avoidable complications allows patients to focus on therapy and rehabilitation rather than managing multiple uncoordinated health issues.
Supporting Emotional and Mental Health
A cancer diagnosis brings significant emotional strain. Anxiety, depression, and stress can interfere with treatment adherence, recovery, and quality of life. Mental health support is therefore a critical component of coordinated care.
Alliance Psychology (https://alliancepsychologyut.com/) provides therapy, psychiatric care, and supportive counseling tailored to individuals navigating cancer treatment. Early engagement in mental health services enables patients to develop effective coping strategies, manage their fears, and maintain motivation throughout therapy.
Primary care providers often serve as the first line in recognizing emotional distress, referring patients to appropriate mental health services, and monitoring the effectiveness of interventions. This continuity ensures that mental health care is integrated seamlessly with medical treatment.
Nutrition, Lifestyle, and Functional Health
Cancer treatment can alter appetite, digestion, and energy levels, making nutrition and lifestyle management key factors in overall outcomes. Primary care providers guide patients in maintaining balanced diets, exercise routines, and sleep hygiene, which support physical resilience and treatment tolerance.
Nutritional counseling and lifestyle interventions are particularly important for patients undergoing chemotherapy or radiation, which can cause fatigue, nausea, and weight fluctuations. Regular guidance helps prevent malnutrition and maintains functional independence.
By addressing lifestyle factors alongside medical treatment, primary care ensures that patients remain active participants in their health journey, enhancing both recovery and long-term wellness.
Coordination With Oncology Teams
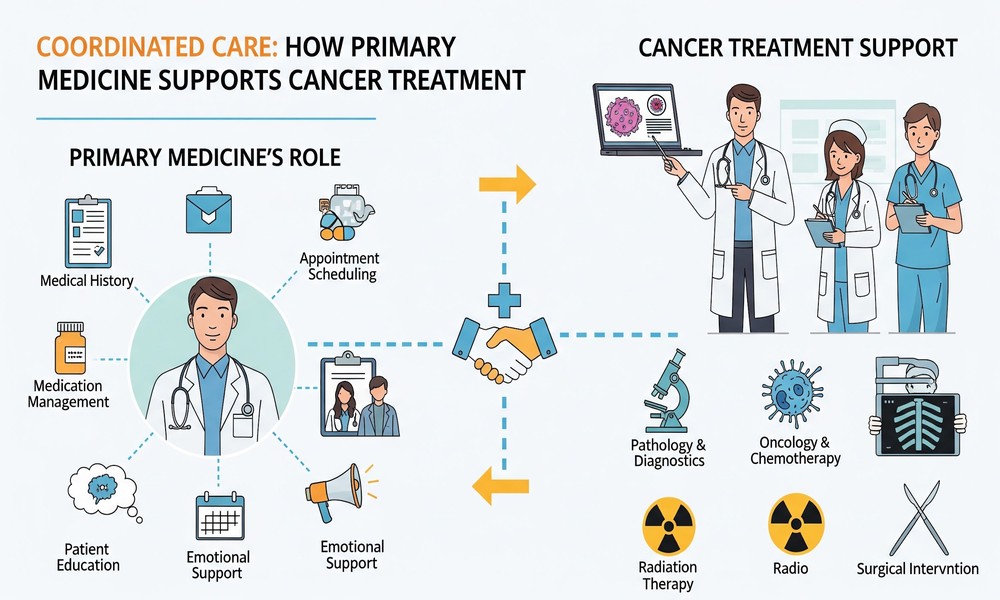
Seamless communication between primary care and oncology specialists is vital. Oncologists focus on cancer-specific treatments, while primary care physicians manage comorbidities, preventive care, and overall health monitoring.
Cancer Center of Southern California provides comprehensive cancer treatment, including surgery, chemotherapy, radiation, and clinical trials. Coordination with primary care providers ensures that therapy is personalized to each patient’s broader health profile, minimizing risks and optimizing recovery.
Shared records, regular updates, and collaborative care planning allow patients to navigate complex treatment schedules without duplicating tests or missing critical interventions. This integrated approach enhances both safety and patient confidence.
Post-Treatment Monitoring and Survivorship
Even after completing cancer therapy, ongoing monitoring is crucial. Survivors may face late effects from chemotherapy or radiation, secondary cancers, and ongoing mental health challenges. Primary care physicians continue to track these risks through regular examinations, lab work, and preventive screenings.
Post-treatment care also includes guidance on lifestyle modification, rehabilitation, and psychological support. Patients benefit from coordinated follow-ups that integrate oncology expertise with general health maintenance, helping them transition from active treatment to long-term wellness.
Alliance Psychology may continue to support emotional resilience, while primary care ensures that survivors maintain optimal health metrics, vaccinations, and preventive screenings.
Patient-Centered Strategies for Holistic Care
Patients often experience better outcomes when care is tailored to their individual needs, rather than fragmented across multiple providers. Personalized care plans account for medical history, treatment goals, lifestyle, and mental health.
Education is another cornerstone: patients who understand potential side effects, warning signs, and recovery milestones are better equipped to advocate for themselves. Providers can guide them in self-monitoring, symptom tracking, and making informed decisions about supportive therapies.
Holistic care models emphasize collaboration between primary care, oncology, and mental health teams, ensuring that treatment addresses the patient’s physical, emotional, and social needs comprehensively.
Preventive Care as a Foundation
Prevention is an ongoing priority, even during active cancer treatment. Vaccinations, screenings, and regular health check-ups reduce the risk of infections, secondary conditions, and delayed detection of new health issues.
Grand Forks Clinic supports this preventive approach by maintaining long-term relationships with patients, tracking trends over time, and coordinating care across specialties. Patients benefit from proactive interventions that strengthen immunity, mitigate complications, and reinforce overall wellness.
This foundation allows cancer therapies to be delivered safely and effectively while preserving quality of life, highlighting the importance of integrating preventive medicine into oncology care.
Conclusion: Strength in Integrated Healthcare
Cancer care is most effective when it is part of a coordinated healthcare network. Primary care physicians, oncologists, and mental health specialists each play unique roles, but collaboration ensures that patients receive comprehensive, patient-centered support.
Through early detection, chronic disease management, mental health support, and post-treatment monitoring, primary care strengthens cancer treatment outcomes and overall patient resilience. Patients who engage in a holistic approach are better equipped to navigate challenges, maintain quality of life, and focus on recovery.
Integrated care not only addresses the disease but also reinforces emotional well-being, functional health, and long-term wellness. By viewing the patient as a whole rather than a single diagnosis, healthcare providers foster confidence, empower patients, and create a sustainable path to recovery and continued health.